Dr. Akshay Jain, MD, FRCPC, FACE, CCD, ECNU, DABIM, DABOM Endocrinologist
Living with diabetes means managing more than just blood sugar. Over time, high blood glucose can silently damage blood vessels and organs, increasing the risk of complications—especially to the heart and kidneys. But the good news? With early interventions, smart medication choices and lifestyle changes, you can protect these vital organs and stay ahead of the curve.
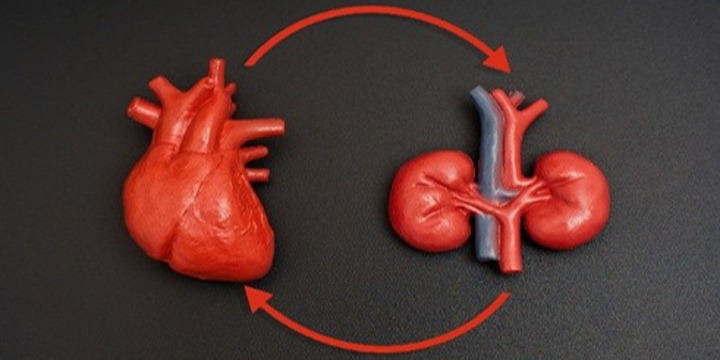
How Diabetes Affects the Heart and Kidneys
Diabetes increases the risk of both cardiovascular disease (CVD) and chronic kidney disease (CKD). Elevated blood sugar can damage the inner lining of blood vessels, leading to inflammation, stiffness, and plaque buildup (atherosclerosis). This increases the risk of heart attacks, strokes and heart failure.
At the same time, high glucose levels can damage the kidneys’ filtering units (glomeruli). Over time, this leads to protein buildup in the urine (albuminuria) and a decline in estimated glomerular filtration rate (eGFR)—markers that signal worsening kidney function. Alarmingly, CKD often progresses without symptoms until it’s advanced.
According to the National Kidney Foundation, diabetes is the number one cause of kidney failure in adults. Meanwhile, people with CKD and diabetes face a much higher risk of dying from cardiovascular causes than reaching dialysis.
Why Albuminuria and eGFR Matter
These are more than just lab values—they’re early warning signals:
- Albuminuria (typically measured as the urine albumin-to-creatinine ratio, or UACR) indicates leaky kidney filters and increased cardiovascular risk—even at low levels.
- eGFR estimates how well your kidneys are filtering blood. A decline over time is a key sign of progressive kidney disease.
Regular screening helps catch problems early, even before symptoms start. Everyone with diabetes should have UACR and eGFR checked at least annually.
Strategies for Protecting Your Heart and Kidneys
1. Control Blood Pressure
Keeping blood pressure below 130/80 mmHg is crucial for both heart and kidney health. RAAS inhibitors (i.e., ACE inhibitors or ARBs) are preferred first-line medications when albuminuria is present, as they lower proteinuria and slow CKD progression.
2. Optimize Blood Sugar—With the Right Tools
While keeping blood sugar in range is essential, how you do it matters:
- SGLT-2 inhibitors (e.g., empagliflozin, dapagliflozin, canagliflozin) not only lower glucose but also reduce the risk of kidney disease progression, heart failure and cardiovascular death.
- GLP-1 receptor agonists (e.g., semaglutide, liraglutide, dulaglutide) improve glucose control, support weight loss, and reduce major cardiovascular events.
- Mineralocorticoid receptor (MR) antagonists (e.g., finerenone), offers added protection by reducing kidney disease progression and heart complications in patients with persistent albuminuria despite RAAS blockers.
3. Lower Cholesterol
Statins are usually recommended for people with diabetes over the age of 40, especially those with additional risk factors. They reduce heart attacks, strokes, and may even have kidney benefits.
4. Embrace Lifestyle Changes
Small changes can have a big impact:
- Exercise regularly (150 min/week of moderate activity).
- Eat a heart-healthy diet, such as the Dietary Approaches to Stop Hypertension (DASH) or Mediterranean diet.
- Reduce sodium intake to support blood pressure control.
- Avoid smoking, which damages blood vessels and accelerates kidney decline.
Common Myths About Kidney and Heart Health in Diabetes
Let’s bust some misconceptions that often lead to delays in treatment or false reassurance.
Myth 1: “I feel fine, so my kidneys and heart must be fine.”
Fact: Kidney disease and heart disease can be silent for years. You may not feel any symptoms until significant damage has occurred. Regular lab tests are the only way to detect problems early.
Myth 2: “If my blood sugar is controlled, I don’t need to worry about my kidneys or heart.”
Fact: While glucose control is vital, it’s not the whole story. Many people with well-controlled diabetes still develop CKD or heart disease. That’s why it’s important to address blood pressure, cholesterol and albuminuria, and to consider medications with proven cardio-renal benefits.
Myth 3: “Once kidney function starts declining, there’s nothing I can do.”
Fact: Not true! With early detection and the right medications (i.e., SGLT-2 inhibitors, RAAS blockers, GLP-1 RAs and MR antagonists), you can slow progression or even stabilize kidney function.
Myth 4: “All diabetes medications are the same.”
Fact: Some newer medications not only lower blood sugar but also protect the heart and kidneys. Talk to your doctor about whether SGLT-2 inhibitors or GLP-1 receptor agonists might be right for you, especially if you have signs of CKD or a history of heart disease.
Myth 5: “Kidney damage only happens if you’re on insulin or have had diabetes for a long time.”
Fact: Kidney damage can occur even in the early years of type 2 diabetes, and sometimes in people who aren’t on insulin. Screening should begin at diagnosis and continue regularly.
Final Thoughts
Kidney and heart complications don’t have to be an inevitable part of diabetes. By focusing on early screening, comprehensive risk management and modern therapies, you can significantly reduce the risk of long-term complications.
Take charge of your health by:
- Keeping tabs on albuminuria and eGFR
- Asking your doctor about SGLT-2 inhibitors, GLP-1 RAs, or MR antagonists
- Managing blood pressure and cholesterol
- Making sustainable lifestyle changes
With the right plan and a proactive mindset, you can protect your heart and kidneys—and live a healthier, longer life with diabetes.
This content is supported by Bayer Inc. The author maintains editorial control over this content. Statements of fact and opinions expressed are those of the author and do not necessarily reflect the views or position of Bayer Inc.